The silent global epidemic of non-communicable diseases (NCDs) has recently caught the world’s attention, of which cancer is a major contributor to disease. Cancer is one of the biggest killers in the 21st century. As the world’s population is ageing in most regions in the world it is predicted that the burden of cancer will continue to increase. There is still a widely held view that cancer only affects those in wealthier regions of the world and the elderly, yet at least half of cancers are diagnosed in developing countries and these carry the greatest burden of premature mortality from cancer.
The leading causes of deaths from NCDs – responsible for 2 out of every 3 deaths globally – are cardiovascular diseases, cancer, respiratory diseases and diabetes. Cancer is a leading cause of death worldwide claiming 8 million lives annually (around 15% of all deaths)1. This varies four-fold across geographical regions, from around 5% in Africa to 20% in the Western Pacific of all deaths worldwide are due to cancer. More than a quarter of all deaths in the UK are due to cancer2.
The growing impact of cancer and other NCDs on global health has placed them on the international agenda. In 2011, NCDs were recognised as a global health priority by Commonwealth Health Ministers at their annual meeting, and by world leaders at the UN High Level Meeting on the Prevention and Control of NCDs. This is only the second High Level Meeting on a health issue convened by the UN General Assembly, following HIV/AIDS, emphasising the threat of NCDs to development worldwide.
Cancer and Ageing
Life expectancy has increased since 1970 on average by 10 years, with a climb to 73 years in women and 67 years in men on average globally. However, although life expectancy has been extended, the number of years lost to disability has also increased; therefore, although people are living longer, they are more likely to be living with disease. The world is witnessing an epidemiological transition from infectious diseases, mainly affecting young children, to chronic diseases in adulthood. Even in the African region, where life expectancy is lower1, this shift is predicted to occur by 20303.
A person’s risk of developing cancer increases with age. The biological process of ageing is itself a risk factor for developing cancer due to accumulation of genetic mutations and cell damage over a lifetime of exposure to carcinogens from lifestyle and environmental factors. As the world’s population continues to age and grow, the burden of cancer will inevitably increase, even if current incidence rates remain the same2. The annual number of new cancer cases is projected to exceed 20 million by 20304, whereas the number of deaths associated with NCDs (in general) are projected to rise substantially by 15% by 20202.
The biological process of ageing is itself a risk factor for developing cancer due to accumulation of genetic mutations and cell damage over a lifetime of exposure to carcinogens from lifestyle and environmental factors
Although cancer is predominantly a disease associated with the elderly, the distribution of cancer worldwide is not exclusive to the old and frail. It is estimated that potentially half of all cancers in developing countries occur in those less than 65 years of age5. Although globally more than two thirds of breast and cervical cancer deaths are estimated to occur in women over 50, more women are dying from breast and cervical cancer at a younger age in low and middle income countries6. Many of the lifestyle factors associated with cancer and other NCDs begin in childhood, and hence prevention efforts targeting young people are extremely important to promote behavioural change that will reduce the risk of these diseases blighting them in later life.
Lifestyle Factors
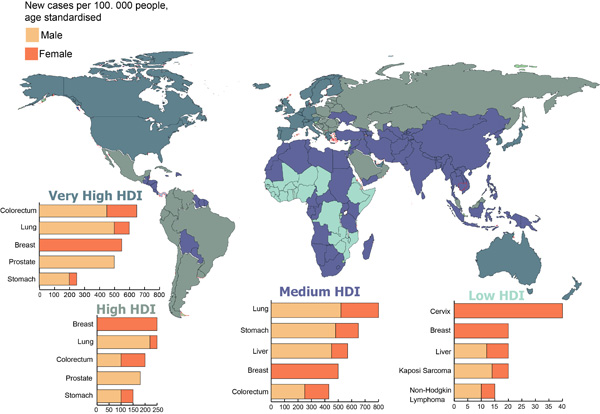
Lung, female breast, colorectal, stomach and liver cancers cause the majority of cancer morbidity and mortality worldwide. There is wide geographical variation in cancer patterns worldwide, depending on the prevalence of underlying risk factors. The major risk factors for cancer include the main four shared behavioural factors for all NCDs; tobacco use, unhealthy diet, insufficient physical activity and the harmful use of alcohol. In the UK the most common cancers diagnosed are breast, lung, colorectum and prostate, and together these cancers account for almost half of the UK’s total2.
Many of the lifestyle factors associated with cancer and other NCDs begin in childhood
Breast cancer has increased in most countries worldwide – cases have more than doubled globally since 1980 – with just over half of these cases now occurring in developing countries6. This increase is only in part explained by population growth and ageing, and the rapid increase in cases seen in low and middle-income countries is thought to be due to the adoption of lifestyle factors, which are associated with higher breast cancer risk as these countries develop2. Approximately 47% of cancer cases and 55% of cancer deaths occur in less developed regions of the world4. Rapid economic growth in many developing countries, accompanied by rapid urbanization, is leading to the adoption of ‘Western’ lifestyle habits and diets and the associated disease burden. Low and middle income countries already bearing the burden of infectious diseases are now facing a double burden from cancer and other NCDs. Cancers that were previously uncommon in these countries are now becoming more prevalent, such as lung, breast and colorectal cancer.
Infectious Diseases
Infectious diseases also contribute to the burden of cancer. Around one in six cancers are caused by chronic infection, most of which are cancers of the cervix, stomach and liver. Around a quarter of new cancer cases in developing countries are attributable to infection compared with less than 10% in developed countries4. The HIV epidemic exacerbates the impact of infection-attributable cancer through weakening of the immune system of those infected, particularly in sub-Saharan Africa that is worst affected. The incidence rates of the cancers Kaposi Sarcoma and Non-Hodgkin Lymphoma, caused by infection with the herpes virus and Epstein Barr virus respectively, are higher in those living with HIV and are most prevalent in low income countries. Access to treatment for HIV and AIDS is steadily improving in many parts of the world enabling those living with HIV to survive for longer, which also means more patients are likely to develop cancer.
There remain many myths surrounding cancer which need to be dispelled. First and foremost, that it is only a problem for wealthy nations with ageing populations. Fatalism associated with cancer also needs to be challenged to mobilise the global community into action against a formidable disease against which much can be done even with limited resources7. One third of all cancer cases are preventable globally, and many more can be treated effectively if detected early. As lifestyle diseases increase, a paradigm shift from health systems that not only save lives but also deliver holistic health care will be required, particularly in low resource settings. However, this will require an input of resources to match the burden of disease as currently less than 3% of development assistance for health is spent on NCDs in low and middle-income countries8.
Scientific research will be crucial in helping to understand the underlying mechanisms leading to development of cancer. Research has already shown that cellular mechanisms in place to prevent tumour growth can slow down the ageing process, but also progress ageing under other circumstances9. Cancer and ageing are two sides of the same coin, and it is a delicate balance between biological mechanisms that keeps us healthy. Further research is likely to not only aid us in controlling cancer, but also in our understanding of the ageing process, in the future10.








